How can you Improve Decisions with VA Compensation Claims?
Applications for veterans Disability Compensation come up against a faulty claims process. We have developed an application method that helps improve poor decisions with flawed Compensation claims processing.
In a previous section, we discussed the flawed application process for Compensation claims that often results in poor decisions or denials. We identified the source of this incompetence and our solutions to getting better decisions. You can read more about the faulty process by going to the subject under the table of contents to the right called "Why Claims Are Handled Poorly."
Here are the conclusions for improving decisions that we drew from our analysis of the faulty process. We will discuss each of these in more detail in this section and then introduce at the end the method we have devised to incorporate these solutions.
- Don't allow VA to own your claim, take responsibility for it
- Don't allow Veterans Service Representatives to use up their time allotment by triggering Duty to Assist
- Make sure the rating team knows the claim is fully developed
- Identify the theory of the claim up front
- Summarize the entire claim
- Organize and index medical records
- Organize, index and correlate all other evidence
- Write an organized, persuasive and thorough lay statement
Understanding VA's Duty to Assist
In 2000 the Veterans Claims Assistance Act (VCAA) was enacted into law, creating a landmark change in the Department of Veterans Affairs' duties to notify and assist claimants for VA benefits. The law is codified into the regulations in Title 38 CFR 3.159. The full text of this section is included at the end of this article.
Prior to the passage of the VCAA, the process of applying for Disability Compensation benefits and Pension benefits was somewhat adversarial. In other words, the claimant had to provide enough evidence to convince VA that the claim was "well grounded" so that VA would assist in developing for further evidence by ordering records and arranging for medical examinations. The courts at that time defined "well grounded" as providing enough evidence so that the claim was considered "plausible." If the claim was not well grounded, VA had the right to reject it.
On the other hand, over the years the Department recognized that outright rejection of an application was not a fair process and so the Department had informally adopted a policy of helping veteran claimants develop their evidence. With the creation of the Court of Appeals for Veterans Claims in 1988 and subsequent decisions from that court, this informal policy of assistance was ruled invalid and VA was prohibited from informally helping to develop evidence.
Recognizing that these court rulings were a detriment to claimants, Congress codified the informal duty to assist process that had been occurring over the years into a formal process under the Veterans Claims Assistance Act of 2000.
Under the new rules, a veteran only had to submit enough information to trigger the duty to assist by submitting a substantially complete claim. A substantially complete application means an application containing:
- The claimant's name;
- His or her relationship to the veteran, if applicable;
- Sufficient service information for VA to verify the claimed service, if applicable;
- The benefit sought and any medical condition(s) on which it is based;
- The claimant's signature; and
- In claims for nonservice-connected disability or death Pension and parents' dependency and indemnity Compensation, a statement of income;
- In supplemental claims, identification or inclusion of potentially new evidence (see §3.2501);
- For higher-level reviews, identification of the date of the decision for which review is sought.
The following was taken from VetsFirst online:
"Once a substantially complete application has been submitted, VA has a second "duty to notify." This time VA has to tell the claimant (1) what information is needed to substantiate the claim, (2) what part of that information VA will try to obtain; and (3) what information that the claimant is responsible for providing to VA. Each time a new issue or claim arises, VA has the same duty to notify the claimant of what information is needed and who (VA or claimant) is responsible for obtaining it.
VA is required to make "reasonable efforts" to obtain a claimant's military service records, VA medical records, and other pertinent federal records without being asked to do so. If a claimant requests assistance in obtaining records from private physicians and hospitals, VA is required to try to obtain those records as well. However, VA is not required to continue to request or wait for records if it determines that the records do not exist or further efforts to obtain the records would be futile. In addition, VA will not pay for obtaining private medical records.
As a practical matter, VA usually can obtain records from government agencies and the military without significant problems. There are situations, however, where VA does not properly request documents or the documents have been lost or destroyed by another agency. VA must inform a claimant of its failure to obtain relevant records. A claimant can and should submit his or her copy of relevant documents even if VA is technically responsible for obtaining the information because the lack of relevant information can result in denial of an otherwise valid claim.
VA is required to schedule a Compensation and Pension (C&P) examination for a claimant at the nearest VA medical center unless there is a good reason for not doing so, such as when an expert is required that is not available at the nearest facility or the examination is with a VA medical contractor. VA, however, does not have to provide a medical examination in all cases. The standard for providing a medical examination is usually not difficult to meet. VA, however, can refuse to provide a VA medical examination unless there is some reasonable possibility that an examination will provide information that could be useful in deciding the claim.
In general, to obtain a C&P examination a claimant needs to show a current medical condition, some evidence of potential connection to service, and that available medical evidence is not sufficient to allow a decision on the claim. In other words, the claimant must first provide some reason for VA to believe that a medical examination would be helpful in resolving the claim. A claimant's own statement that his or her symptoms have continued since service or a previous medical examination report can be enough of a reason.
Should VA schedule a medical examination, a claimant has a duty to report for the examination. In most cases, if the claimant does not show up for an examination, the claim(s) associated with that examination can be denied without further development. There are some reasons for failing to show for a scheduled examination, such as illness or urgent family emergency, that can be excused. Even so, claimants should make every effort to reschedule an examination in advance to avoid problems.
Once VA has gathered all the reasonably obtainable information, including information submitted by the claimant, VA must decide whether or not to grant an award of benefits. In making that decision, VA must consider three other duties owed to the claimant: (1) duty to identify inferred claims, (2) duty to consider all reasonable legal theories, and (3) duty to maximize benefits. In other words, VA has several duties to apply the rules to the facts in a case in whatever way provides the most generous benefits allowed by the law.
These duties do not mean that VA has to look at every possible combination of rules and facts that may be even remotely possible. VA, however, has to review the entire record and apply the applicable provisions of law that are reasonably raised by the evidence. In addition, whether or not new claims are identified, VA must also review the diagnostic codes for the code or combination of codes that results in the highest benefit for the claimant.
Overall, in creating the duty to assist Congress recognized that VA raters are better trained and more experienced with the rules for obtaining benefits than the average claimant. VA must look for claims and grant awards based on all the evidence in the C-file whether or not the claimant asked for the specific benefit. This is a very good reason for claimants to provide as much information as possible when submitting applications or responding to VA requests."
Unfortunately, duty to assist makes it too easy for veterans to submit applications. What we mean by this is that the typical veteran claimant or the survivor claimant puts his or her full trust in the capabilities of the Department to adequately develop the claim for a decision. The assumption is that the Veteran Service Representatives in the Regional Office will do the best job possible for developing evidence and provide the best decision under the circumstances. As we have discussed in the previous section on the flaws in the claims processing model, PUTTING YOUR ENTIRE TRUST IN VA TO DEVELOP A CLAIM FOR A DECISION IS A BAD IDEA.
Don't Allow VA to Own Your Claim, Take Responsibility for It
VA apologists would argue that the purpose of the Department's paternalistic assistance with duty to assist is to not put a burden on the claimant, especially for incurring out-of-pocket costs. The issue is that the veteran or survivor simply can't afford to pay for preparation of an application. Unfortunately, as we have pointed out, the claim system is flawed. Not only that, we believe that employees in the veterans service center are somewhat jaded. They see the same questionable claims with little evidence, coming through every day and it probably causes employees to feel some reluctance for development knowing that many of these claims are meritless.
As a result, the veteran or survivor must defend himself or herself against adverse actions that the rating team in the Regional Office will take possibly because of this attitude. If you really want to get a favorable decision with the best possible disability rating, you have to put some time and money into it. In reality, that's the way it works.
It's not that the people in the Regional Office are deliberately trying to take your benefits away. On the contrary, they rightly believe they are doing their job by questioning evidence that appears to be suspicious or lacking. Even though they are paid to be advocates for the veteran, it often appears to these people who work for VA – from many years of experience –that many veterans are trying to get something for nothing. And in many cases this is probably true. VA employees probably act adversely because of their experience in trying to prevent someone from getting a benefit to which that person is not entitled.
The suspicion from the Regional Office is not due to policy. Regulations prohibit adjudicators from exhibiting bias. It is due to questionable evidence from many years of experience dealing with this issue. One important strategy to win the confidence of the development and rating team is to submit a claim that commands their respect. You do this through
- detailed and well-argued lay statements,
- credible and probative medical evidence that you provide yourself
- well-reasoned and documented medical opinions that you provide yourself and
- support from credible medical literature where necessary
We will discuss in more detail further on in this section how to go about gathering and creating the material for a persuasive, well-developed claim.
Don't Allow Veterans Service Representatives to Use up Their Time Allotment by Triggering Duty to Assist
It is absolutely important to avoid duty to assist at all costs. As we mentioned in the previous section concerning the flaws in the application process, Veteran Service Representatives in the Regional Office are only given so much time to adjudicate a claim. Much of the time devoted to the adjudication is a result of duty to assist. Requesting records, sending out notices, requesting records again, arranging for medical evaluations and all of the other necessary actions to develop a claim for decision take up all the allotted time.
The remaining six important directives that we discuss below are necessary for you to follow in order to help those service representatives use their allotted time in a way that will provide a more positive decision for your claim instead of their wasting valuable allotted time on developing for evidence that you have already provided.
Make Sure the Rating Team Knows the Claim Is Fully Developed
Sometime around 2012 VBA came up with an excellent idea called the "Fully Developed Claim." Prior to this, VA's duty to assist was absolute, based on the Veterans Claims and Assistance Act of 2000. Duty to assist could not be avoided.
The fully developed claim allows an applicant to disavow his or her right to duty to assist and to pass the claim with all of the attending evidence directly to the decision-maker. This avoids months of records requests, unnecessary notices and other activities that are not needed for a claim that is complete and ready for a decision.
Fully developed claims allow processing teams in the Regional Office to meet their time constraints under the processing model. It is a win-win for the employee and for the applicant. New EZ forms were developed for this purpose and currently these are the forms that should be used for any application.
We don't have any specific statistics, but based on empirical evidence, hardly any applicants are submitting Compensation claims that are fully developed. There are probably 2 reasons for this. First, a claimant who is submitting an application for the first time – without any assistance from someone who is experienced, will likely not understand how to do a fully developed claim. Even though instructions are on the form – and they are very good instructions – the process is complicated and intimidating.
Second, if a claimant is using the assistance of an accredited representative of a veterans service organization, that representative may very well know how to do a fully developed claim but will not take the time to do it. Service officers of VSOs are paid by how much paperwork they can generate in a given month or year. If they don't produce, they don't have a job. Putting together a fully developed claim takes a great deal of time, but doesn't result in any more applications than submitting a form that is not fully developed and takes only a few minutes. Veterans service officers often have people waiting for their assistance and they don't have time for anything else other than filling out forms.
We provide you information further on in this section on the method we have designed to notify the adjudicators in the Regional Office that the claim is actually fully developed even though the application form is for a fully developed claim. What happens is if the service representatives in the Regional Office are not made aware that all the evidence has been submitted for a decision – even though the application says that – they will automatically remove the claim from the fully developed claims track and put it on the standard claims track and start developing under duty to assist. They very seldom see fully developed claims for Disability Compensation and as a result they employ a knee-jerk reaction to ignore real live fully developed claims and not follow the proper procedure for such claims.
Identify the Theory of the Claim up Front
Oftentimes, for a complex claim with a number of disability issues, there is an underlying theory of the claim that produces those disabilities. For example, a back injury in service can lead to all kinds of secondary disabilities such as stenosis, sciatica, neuropathy pain, weakness and static pain. The application for Disability Compensation, VA Form 21-526 EZ, does not provide enough space on the form to develop a theory or multiple theories of the claim. On the contrary, the application focuses entirely on the disability issues and treats them as separate issues instead of relating to a single event or events that caused them.
Under duty to assist, the adjudicator is supposed to infer a theory of the claim from the evidence. The problem here is that for complex claims the theory is not always evident and the other problem is that due to time constraints adjudicators rarely review all of the medical evidence and so they have no opportunity to see the "big picture."
It is essential that you identify the theory of the claim right up front and put it in the adjudicator' s face. If you allow the adjudicator to determine his or her own theory of the claim you have just gone down a path that you cannot return from. In other words, once the rating team in the Regional Office have determined what they think the theory of the claim is, they will not deviate from that course no matter how much new evidence you give them to show that they are on the wrong path. As a result, a denial of your claim is often inevitable no matter what you try to do to forestall it.
Summarize the Entire Claim
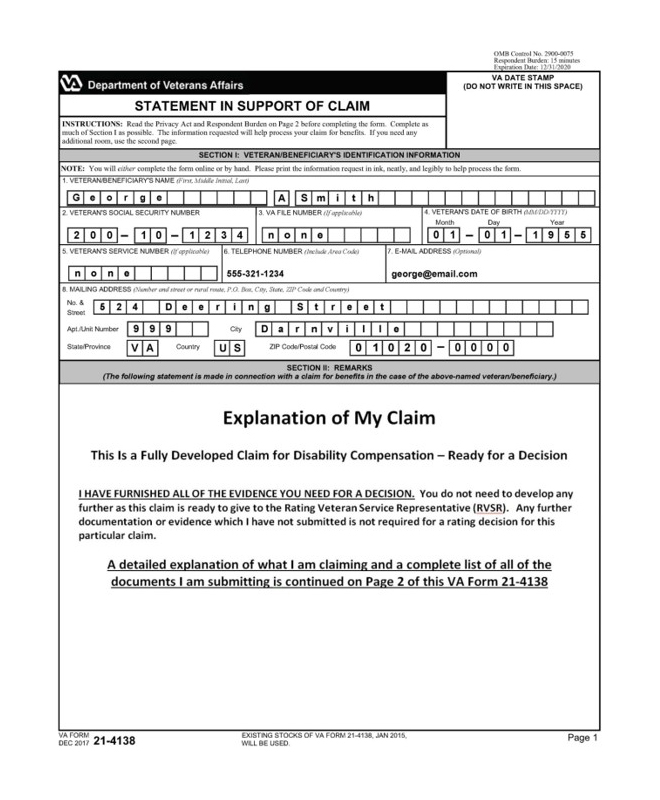
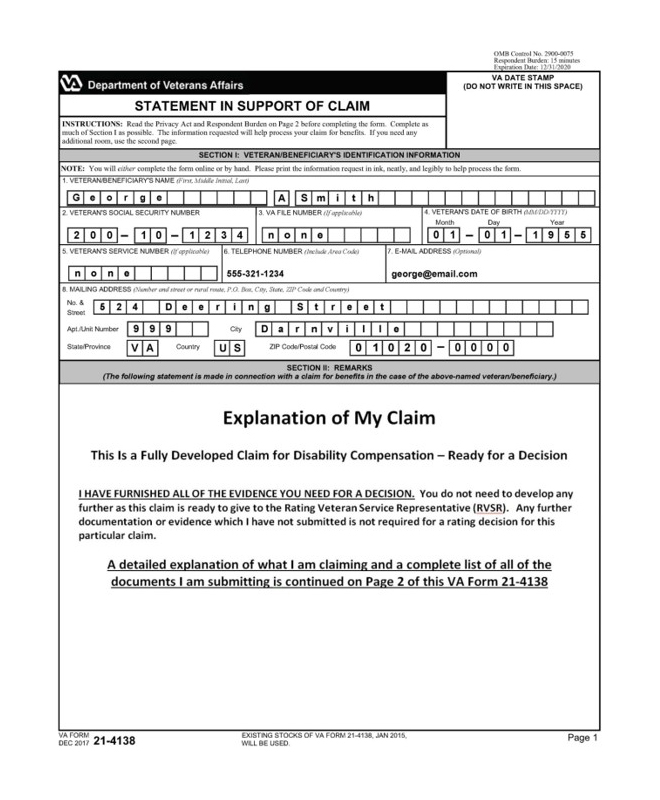
Summarizing the entire claim on a separate VA Form 21-4138 allows you to bypass the restrictive entry options on the application form itself – VA Form 21-526 EZ. You will have ample space to discuss and identify all of the issues pertaining to your claim by tying together all of the evidence and identifying the theory of the claim. Using this approach, you have enough space to detail several paragraphs of information.
The key to any summary is not to overdo it. Providing too much information is just as bad as not providing enough. If you overload the rating team with pages and pages of summary, they will likely not read it as they are under time constraint. On the other hand, if you are too sketchy, they will not understand what you are claiming. We recommend no more than two or three paragraphs. This means you must work very hard to communicate your claim in as few words as possible. Writing such a summary can often be one of the more challenging aspects of filing an application.
Organize and Index Medical Records
Under existing rules for adjudicating claims, Veteran Service Representatives must review all of the pertinent evidence that relates to that claim. In reality, we have discovered this just doesn't happen. For those claims where there is a great deal of medical evidence to pour through, that evidence is never thoroughly reviewed. As a result of this, bad decisions and denials are often forthcoming. This is because in lieu of reviewing evidence or medical literature that is submitted with the claim, the service representative will take a shortcut by ordering a medical exam and an opinion.
Practically all medical examinations and opinions ordered by VA are through 5 large national contractors who in turn contract with physicians assistants and nurse practitioners and sometimes medical doctors to do these examinations. This system is flawed as well. Examiners are only given a certain amount of time to do the examination and in most cases, they are not even asked to write adequate opinions but simply to check off a number of boxes. This system is probably in violation of the intent of the regulations and someday may be challenged in court, but in the meantime we have to put up with it.
In all cases, we attempt to bypass this shortcut system for reviewing medical records by sorting out only those records that apply and then identifying them with a cover page and a table of contents that describes what is in them. Thus a claims file that may have 800 pages of medical records, can be organized and indexed properly so that only about 10 or 20 of those pages that are necessary for a decision are presented to the adjudicator. Sometimes, we even summarize the record for them in a few paragraphs and then refer to the actual medical record file itself.
Organize, Index and Correlate All Other Evidence
The same method that we described in the subsection above is used for all other evidence. This includes personnel records, pertinent medical literature, personally procured DBQs and personally procured medical opinions and any other evidence necessary for a fully developed claim.
Just as with medical records, this material must be organized with tables of content and cover pages identifying what it is and a short description on the cover page pertaining to the nature of the evidence.
Write an Organized, Persuasive and Thorough Lay Statement
A well-written and detailed personal lay statement is often essential to winning an award. A lay statement is a narrative of your claim which describes in detail the incident that was incurred in service, the history since discharge pertaining to the medical repercussions from that incident and a description of the current disability. Lay statements can come from the claimant or from fellow soldiers who were present and observed the particular incident or from a spouse or family member who has observed symptoms over the years and verifies continuity of those symptoms.
It's important to know that a lay statement cannot contain a medical nexus opinion unless the person writing the statement is a licensed medical provider and is competent to provide that opinion. However, this does not preclude the person who is writing this statement from testifying of known facts from a source that is qualified to support a nexus opinion. For example the claimant can testify of diagnoses or other conditions that were given to the claimant either orally by treating physicians or through medical records that no longer exist.
The claimant can also testify to opinions that were offered by treating medical providers. In addition, the claimant can provide substantial evidence from competent medical literature that supports his or her assertions for service connection or a disability rating decision. When using medical literature evidence, the lay statement should point out why that literature supports the service connection rating or disability rating.
Lay Evidence in a VA Claim has zero evidentiary value if the adjudicator in the Regional Office or the BVA Judge does not think it is credible and competent. When considering lay evidence, the Board or adjudicator should determine whether the veteran's disability is the type of disability for which lay evidence is competent. See Jandreau, 492 F.3d at 1377. If the disability is of the type for which lay evidence is competent, the adjudicators must weigh that evidence against the other evidence of record in making its determination regarding the existence of a service connection. Buchanan, 451 F.3d at 1334-37. Here are the criteria for determining that.
- It must determine if the lay evidence is competent and provides an adequate explanation of determination (Jandreau v. Nicholson, 492 F.3d 1372 Fed. Cir. 2007)
- It must weigh the lay evidence against other evidence to make a determination of its value on the claim (Buchanan v. Nicholson, 451 F.3d 1331, 1334-1337 Fed. Cir. 2006)
- It must make a credibility determination as to whether the evidence supports a finding of service connection and a continuity of symptomology (Barr v. Nicholson, 21. Vet App. 303 2007)
The Senior Veterans Service Alliance Application Method
At the Senior Veterans Service Alliance, we have devised a method to incorporate all of the actions discussed above. There is too much detail and too many moving pieces with our method to present it here. There are also a number of special forms that we have designed to incorporate this method. Here is an example of the first two pages of one of these forms which is a modified VA Form 21-4138.
Title 38 CFR §3.159 Department of Veterans Affairs assistance in developing claims.
(a) Definitions. For purposes of this section, the following definitions apply:
(1) Competent medical evidence means evidence provided by a person who is qualified through education, training, or experience to offer medical diagnoses, statements, or opinions. Competent medical evidence may also mean statements conveying sound medical principles found in medical treatises. It would also include statements contained in authoritative writings such as medical and scientific articles and research reports or analyses.
(2) Competent lay evidence means any evidence not requiring that the proponent have specialized education, training, or experience. Lay evidence is competent if it is provided by a person who has knowledge of facts or circumstances and conveys matters that can be observed and described by a lay person.
(3) Substantially complete application means an application containing:
(i) The claimant's name;
(ii) His or her relationship to the veteran, if applicable;
(iii) Sufficient service information for VA to verify the claimed service, if applicable;
(iv) The benefit sought and any medical condition(s) on which it is based;
(v) The claimant's signature; and
(vi) In claims for nonservice-connected disability or death Pension and parents' dependency and indemnity Compensation, a statement of income;
(vii) In supplemental claims, identification or inclusion of potentially new evidence (see §3.2501);
(viii) For higher-level reviews, identification of the date of the decision for which review is sought.
(4) For purposes of paragraph (c)(4)(i) of this section, event means one or more incidents associated with places, types, and circumstances of service giving rise to disability.
(5) Information means non-evidentiary facts, such as the claimant's Social Security number or address; the name and military unit of a person who served with the veteran; or the name and address of a medical care provider who may have evidence pertinent to the claim.
(b) VA's duty to notify claimants of necessary information or evidence. (1) Except as provided in paragraph (3) of this section, when VA receives a complete or substantially complete initial or supplemental claim, VA will notify the claimant of any information and medical or lay evidence that is necessary to substantiate the claim (hereafter in this paragraph referred to as the "notice") In the notice, VA will inform the claimant which information and evidence, if any, that the claimant is to provide to VA and which information and evidence, if any, that VA will attempt to obtain on behalf of the claimant. The information and evidence that the claimant is informed that the claimant is to provide must be provided within one year of the date of the notice. If the claimant has not responded to the notice within 30 days, VA may decide the claim prior to the expiration of the one-year period based on all the information and evidence contained in the file, including information and evidence it has obtained on behalf of the claimant and any VA medical examinations or medical opinions. If VA does so, however, and the claimant subsequently provides the information and evidence within one year of the date of the notice in accordance with the requirements of paragraph (b)(4) of this section, VA must readjudicate the claim.
(Authority: 38 U.S.C. 5103)
(2) If VA receives an incomplete application for benefits, it will notify the claimant of the information necessary to complete the application and will defer assistance until the claimant submits this information.
(Authority: 38 U.S.C. 5102(b), 5103A(3))
(3) No duty to provide the notice described in paragraph (b)(1) of this section arises:
(i) Upon receipt of a supplemental claim under §3.2501 within one year of the date VA issues notice of a prior decision;
(ii) Upon receipt of a request for higher-level review under §3.2601;
(iii) Upon receipt of a Notice of Disagreement under §20.202 of this chapter; or
(iv) When, as a matter of law, entitlement to the benefit claimed cannot be established.
(Authority: 38 U.S.C. 5103(a), 5103A(a)(2))
(4) After VA has issued a notice of decision, submission of information and evidence substantiating a claim must be accomplished through the proper filing of a review option in accordance with §3.2500 on a form prescribed by the Secretary. New and relevant evidence may be submitted in connection with either the filing of a supplemental claim under §3.2501 or the filing of a Notice of Disagreement with the Board under 38 CFR 20.202, on forms prescribed by the Secretary, and election of a Board docket that permits the filing of new evidence (see 38 CFR 20.302 and 20.303).
(c) VA's duty to assist claimants in obtaining evidence. VA has a duty to assist claimants in obtaining evidence to substantiate all substantially complete initial and supplemental claims, and when a claim is returned for readjudication by a higher-level adjudicator or the Board after identification of a duty to assist error on the part of the agency of original jurisdiction, until the time VA issues notice of a decision on a claim or returned claim. VA will make reasonable efforts to help a claimant obtain evidence necessary to substantiate the claim. VA will not pay any fees charged by a custodian to provide records requested. When a claim is returned for readjudication by a higher-level adjudicator or the Board after identification of a duty to assist error, the agency of original jurisdiction has a duty to correct any other duty to assist errors not identified by the higher-level adjudicator or the Board.
(1) Obtaining records not in the custody of a Federal department or agency. VA will make reasonable efforts to obtain relevant records not in the custody of a Federal department or agency, to include records from State or local governments, private medical care providers, current or former employers, and other non-Federal governmental sources. Such reasonable efforts will generally consist of an initial request for the records and, if the records are not received, at least one follow-up request. A follow-up request is not required if a response to the initial request indicates that the records sought do not exist or that a follow-up request for the records would be futile. If VA receives information showing that subsequent requests to this or another custodian could result in obtaining the records sought, then reasonable efforts will include an initial request and, if the records are not received, at least one follow-up request to the new source or an additional request to the original source.
(i) The claimant must cooperate fully with VA's reasonable efforts to obtain relevant records from non-Federal agency or department custodians. The claimant must provide enough information to identify and locate the existing records, including the person, company, agency, or other custodian holding the records; the approximate time frame covered by the records; and, in the case of medical treatment records, the condition for which treatment was provided.
(ii) If necessary, the claimant must authorize the release of existing records in a form acceptable to the person, company, agency, or other custodian holding the records.
(Authority: 38 U.S.C. 5103A(b))
(2) Obtaining records in the custody of a Federal department or agency. VA will make as many requests as are necessary to obtain relevant records from a Federal department or agency. These records include but are not limited to military records, including service medical records; medical and other records from VA medical facilities; records from non-VA facilities providing examination or treatment at VA expense; and records from other Federal agencies, such as the Social Security Administration. VA will end its efforts to obtain records from a Federal department or agency only if VA concludes that the records sought do not exist or that further efforts to obtain those records would be futile. Cases in which VA may conclude that no further efforts are required include those in which the Federal department or agency advises VA that the requested records do not exist or the custodian does not have them.
(i) The claimant must cooperate fully with VA's reasonable efforts to obtain relevant records from Federal agency or department custodians. If requested by VA, the claimant must provide enough information to identify and locate the existing records, including the custodian or agency holding the records; the approximate time frame covered by the records; and, in the case of medical treatment records, the condition for which treatment was provided. In the case of records requested to corroborate a claimed stressful event in service, the claimant must provide information sufficient for the records custodian to conduct a search of the corroborative records.
(ii) If necessary, the claimant must authorize the release of existing records in a form acceptable to the custodian or agency holding the records.
(Authority: 38 U.S.C. 5103A(b))
(3) Obtaining records in Compensation claims. In a claim for Disability Compensation, VA will make efforts to obtain the claimant's service medical records, if relevant to the claim; other relevant records pertaining to the claimant's active military, naval or air service that are held or maintained by a governmental entity; VA medical records or records of examination or treatment at non-VA facilities authorized by VA; and any other relevant records held by any Federal department or agency. The claimant must provide enough information to identify and locate the existing records including the custodian or agency holding the records; the approximate time frame covered by the records; and, in the case of medical treatment records, the condition for which treatment was provided.
(Authority: 38 U.S.C. 5103A(c))
(4) Providing medical examinations or obtaining medical opinions. (i) In a claim for Disability Compensation, VA will provide a medical examination or obtain a medical opinion based upon a review of the evidence of record if VA determines it is necessary to decide the claim. A medical examination or medical opinion is necessary if the information and evidence of record does not contain sufficient competent medical evidence to decide the claim, but:
(A) Contains competent lay or medical evidence of a current diagnosed disability or persistent or recurrent symptoms of disability;
(B) Establishes that the veteran suffered an event, injury or disease in service, or has a disease or symptoms of a disease listed in §3.309, §3.313, §3.316, and §3.317 manifesting during an applicable presumptive period provided the claimant has the required service or triggering event to qualify for that presumption; and
(C) Indicates that the claimed disability or symptoms may be associated with the established event, injury, or disease in service or with another service-connected disability.
(ii) Paragraph (4)(i)(C) could be satisfied by competent evidence showing post-service treatment for a condition, or other possible association with military service.
(iii) For requests to reopen a finally adjudicated claim received prior to the effective date provided in §19.2(a) of this chapter, this paragraph (c)(4) applies only if new and material evidence is presented or secured as prescribed in §3.156.
(iv) This paragraph (c)(4) applies to a supplemental claim only if new and relevant evidence under §3.2501 is presented or secured.
(Authority: 38 U.S.C. 5103A(d))
(d) Circumstances where VA will refrain from or discontinue providing assistance. VA will refrain from providing assistance in obtaining evidence for a claim if the substantially complete application for benefits indicates that there is no reasonable possibility that any assistance VA would provide to the claimant would substantiate the claim. VA will discontinue providing assistance in obtaining evidence for an initial or supplemental claim if the evidence obtained indicates that there is no reasonable possibility that further assistance would substantiate the claim. Circumstances in which VA will refrain from or discontinue providing assistance in obtaining evidence include, but are not limited to:
(1) The claimant's ineligibility for the benefit sought because of lack of qualifying service, lack of veteran status, or other lack of legal eligibility;
(2) Claims that are inherently incredible or clearly lack merit; and
(3) An application requesting a benefit to which the claimant is not entitled as a matter of law.
(Authority: 38 U.S.C. 5103A(a)(2))
(e) Duty to notify claimant of inability to obtain records. (1) If VA makes reasonable efforts to obtain relevant non-Federal records but is unable to obtain them, or after continued efforts to obtain Federal records concludes that it is reasonably certain they do not exist or further efforts to obtain them would be futile, VA will provide the claimant with oral or written notice of that fact. VA will make a record of any oral notice conveyed to the claimant. For non-Federal records requests, VA may provide the notice at the same time it makes its final attempt to obtain the relevant records. In either case, the notice must contain the following information:
(i) The identity of the records VA was unable to obtain;
(ii) An explanation of the efforts VA made to obtain the records;
(iii) A description of any further action VA will take regarding the claim, including, but not limited to, notice that VA will decide the claim based on the evidence of record unless the claimant submits the records VA was unable to obtain; and
(iv) A notice that the claimant is ultimately responsible for providing the evidence.
(2) If VA becomes aware of the existence of relevant records before deciding the claim, VA will notify the claimant of the records and request that the claimant provide a release for the records. If the claimant does not provide any necessary release of the relevant records that VA is unable to obtain, VA will request that the claimant obtain the records and provide them to VA.
(Authority: 38 U.S.C. 5103A(b)(2))
(f) For the purpose of the notice requirements in paragraphs (b) and (e) of this section, notice to the claimant means notice to the claimant or his or her fiduciary, if any, as well as to his or her representative, if any.
(Authority: 38 U.S.C. 5102(b), 5103(a))
(g) The authority recognized in subsection (g) of 38 U.S.C. 5103A is reserved to the sole discretion of the Secretary and will be implemented, when deemed appropriate by the Secretary, through the promulgation of regulations.
(Authority: 38 U.S.C. 5103A(g))
[66 FR 45630, Aug. 29, 2001, as amended at 73 FR 23356, Apr. 30, 2008; 84 FR 169, Jan. 18, 2019]
Please refer to the table of contents in the top right column of this page for more topics on VA Disability Compensation.
Find Help in Your Area · Veterans Benefits · Resources · Contact Us

TABLE OF CONTENTS
Disability Compensation
- What is Compensation
- Eligibility for Compensation
- Entitlement for Compensation
- Income Rating Levels
- Presumptive Service-Connected
- Direct Service-Connected
- Secondary Service-Connected
- Common Compensation Claims
- Claims Taking Too Long
- Shorten Claim Decisions
- Options for Bad Decisions
- Claimant Dies before Decision
- Determining Disability Ratings
- Examples of Claims
- Aid & Attendance Allowance
- Other Benefits for Claimants
How to Apply Book

How to Apply for VA Benefits for Veterans and Their Survivors
This 2024 Edition provides detailed instructions on how to submit claims for benefits through the Department of Veterans Affairs new intake center and uses the successful "Fully Developed Claim Process" for faster and better decisions. View the Book...
Navigation
Resources
- About Accreditation & Fees
- Accreditation Study Materials
- CLE to Maintain VA Accreditation
- Correcting Your Military Discharge
- Find Home Care / Assisted Living
- Find Hospice Care
- Find Medical Alert
- Help finding a LTC Facility
- Help with Care Management
- Help with Elder Law
- Help with Estate Planning
- Help with Disputes / Mediation
- Help with Financial Planning
- Help with Medicaid Planning
- Help with Tax Planning
- Informal Claims / Effective Dates
- Service Connected Disabilities
- State VA Nursing Homes
- VA Aid and Attendance Benefit
- VA Burial Benefits
- VA Healthcare System
- VA Help - Surviving Spouse
- VA Home Renovation Grants
- VA Long Term Care Benefits
- VA Pays Family for Eldercare
- VA Regional Offices
VA Forms

This section provides downloadable files of the most commonly used VA Forms for senior veterans seeking benefits from the Department of Veterans Affairs. View the Forms...
Become a Member of the Senior Veterans Service Alliance

Become a member of the SVSA and help our organization support the needs of senior veterans who served their country in a time of need. Learn more about the benefits of membership.